

Time overruns, inadequate management information, lack of discipline, and an unprofessional improvement culture: managing an operating room complex (ORC) is not exactly easy. Here we explain how the TIPOT planning philosophy can take you to ideal operations planning in seven steps – and directly to an OR culture of excellence.
A tense atmosphere just doesn’t cut it
With daily uncertainties rife, OR surgeons and managers often engage in an emotional balancing act between safety and quality of care, on the one hand, and staff deployment and capacity, on the other. A dangerous situation, say a couple of orthopaedists in The Hague. ‘A tense atmosphere just doesn’t cut it.’ With this at the back of our mind, and drawing on our experience and expertise, we developed a philosophy where production and culture in the ORC go hand in hand.
The core values of the hospital and the ORC play a decisive role in the choices made by ORC management. Therefore, describe these core values in detail and explain how they manifest themselves in practice.
In addition, define the meaning of essential terms such as start of day, end of day, lunch, OR staffing, and production. Make a clear summary of all this information so it can be communicated to stakeholders. Discuss this summary with everyone involved in the ORC and list all the rules, including their advantages and disadvantages.
The core value of efficiency means that patients wait in the holding area for 60 minutes so no time is lost when the operating room becomes available. But as a core value, wouldn’t it be better to put the patient first? To move the patient in a smooth line from the unit via the operation to the recovery room – with the same employee available for this patient through the whole OR process.
Make summaries of all OR data (times, production, qualities, etc.) over the past year per specialist group. Assess the outcome based on the findings from step 1. Discuss the results and effects per specific surgeon based on patient characteristics with those involved in the ORC. Start with the surgeons; they play the most decisive role.
We prepared this summary for nine specialist groups in nine hospitals. We found that all groups start the day late (average of 13 minutes), end the day early (average of 18 minutes), and take too much patient turnover time (average of 4 minutes more than planned per patient). In addition, too much time was scheduled per operation: an excess of 16 minutes on average. Regarding the rules and definitions established by the hospital itself, we discovered more than 50 minutes of unused OK time per day.
As a planner or manager, spend a couple of days observing at the ORC to get a real feel for the story behind the numbers. This will also give you the opportunity to address questions directly to the people on the floor and exchange feedback.
When we spent some time observing the ORC, we heard things like: ‘Oh well, it’s only the 16th time this week that this surgeon got to the wrong place.’; ‘Every morning it’s a cat-and-mouse game between the anaesthesiologist and the surgeon.’; ‘With all our overtime, you could easily hire more hands.’; ‘If I have nothing to do for the last hour of the day, I must be working too hard.’
And we saw everything imaginable. Surgeons who – against all the rules – wear earrings, use smartphones, and wear their own shoes during operations. But what really stood out was the lack of motivation. Staff at different ORCs indicated that the management was not very good at addressing problems. As a result, people had become cynical and nonchalant. We found that alarming, because such behaviour goes against the desired professional, safe, and open culture.
Many ORCs plan on the basis of historical data. But that is not the best way, because it makes people dependent on timekeeping by an available OR assistant. Moreover, if the wrong time is entered in the system, it is carried over to the following planning round. And a database is not able to assess specific patient characteristics, such as obesity status and flexibility, which can influence operation time. That is why everything needs to be carefully coordinated with the responsible surgeon for each operation.
A data analysis that we conducted at nine ORCs shows that an average of 100 minutes per operating room are left open every day. Planners indicate that this is because they want to be ‘safe’ and ‘realistic’ in their assessment, which means rounding up the indicated operation times. And since they want employees to be able to go home on time at the end of the day, they prefer avoiding time overruns. The planning software makes it impossible to be flexible to specific patient characteristics. Because of rigid and risk-adverse planning, many operations are finished with plenty of time to spare, leaving the operating room vacant. This way of working has serious consequences for patients (waiting times), quality of care (lack of focus), and the finances (lost income) of hospitals and specialists. Taking action to fix the problem therefore also has serious consequences.
Time overruns and waiting time can arise even when running at full capacity (see figure 1). Staffing levels or capacity utilization rates therefore do not provide the best management information. TIPOT does. TIPOT stands for time-out procedure, wheeling in, positioning, wheeling out, and transfer to hospital bed. All these times (shown in red in figure 2) are standardized per type of operation and anaesthesiology. Turnover time spans a fixed number of minutes that is realistically measured and recorded. The net operating time is the only variable factor, depending on patient, operation, and surgeon. And it’s the surgeon who says how long that takes.
We call the sum of productive OR time the utilization time. TIPOT time-keeping is highly accurate, which makes tighter planning possible. And higher capacity utilization – without any change in staffing level – can be achieved as well.
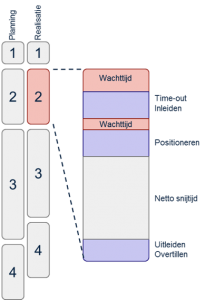
Figure 1: TIPOT provides clarity on lost operating time
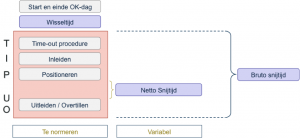
Figure 2: TIPOT illustrated
Discuss how you plan to introduce TIPOT. In any case, start by gaining some experience with it. For example, calculate and set down the TIPOT components of the gross operating time (see figure 2). And in the planning, focus on the capacity utilization rate. Ensure that the planner and surgeon work together closely. After all, the net operating time varies according to specific patient characteristics, which are input by the surgeon. Careful teamwork improves planning quality and ensures good post-evaluation opportunities. Talk to the people involved about their professionalism and consequences of the improvements on the strength of their own core values.
The TIPOT method is only effective if controlled and monitored daily, on the basis of facts. Data analysis and the observation days often show that compliance with rules and with arrangements between colleagues has room for improvement. When asked whether this compliance is enforced, the answer is often: ‘We address this every month at our OR management meeting.’ But this way of working is not effective: incidents are either too numerous or have already been forgotten by that time, the people directly involved are not at that meeting, and the connection between an incident and the steps towards improvement gets lost.
This makes it important for the whole team to assess the OR process every day with a view to the planning and the things that go right or wrong. This takes less than 10 minutes per OR programme. Organize a special meeting for more serious incidents. Direction and culture are the responsibility of the entire ORC management. And yet, professional feedback between everyone on the basis of qualitative and quantitative results is part of a healthy culture of accountability.
For nine specialist groups in nine hospitals, planning according to the TIPOT philosophy unlocked improvement potential of more than 15 per cent of the capacity utilization rate per operating room per day. That is an average of one operation a day or an equal saving in staff deployment: either €1,000,000 more in income or €300,000 less in spending. We find the shorter waiting list for patients and the pleasant and efficient atmosphere the most important result, one which can be ensured through continued steering and leadership…and by celebrating success.
Bespreek hoe u TIPUO gaat invoeren. Zorg in ieder geval dat u er eerst ervaring mee opdoet. Bereken bijvoorbeeld de TIPUO-onderdelen van de bruto snijtijd (zie afbeelding 2) en leg deze vast. En leg bij de planning de focus op de benuttingsgraad. Laat de planner en de operateur nauw samenwerken. De netto snijtijd varieert immers door specifieke patiëntkarakteristieken die de operateur aandraagt. Zorgvuldig samenwerken verbetert de kwaliteit van de planning én zorgt voor goede evaluatiemogelijkheden achteraf. Spreek betrokkenen vanuit de (eigen) kernwaarden aan op professionaliteit en de consequenties van verbeteringen.
De TIPUO-methodiek heeft alleen effect als er daadwerkelijk gestuurd wordt, dagelijks en op basis van feiten. Vaak blijkt uit de data-analyse en de observatiedagen dat naleving van afspraken en sturen op bestaande afspraken voor verbetering vatbaar is. Op onze vraag of dit sturen werkelijk gebeurt, is het antwoord vaak: ‘Dit doen we elke maand in het OK-bestuur’. Deze werkwijze is echter niet effectief omdat incidenten al vergeten of te talrijk zijn, direct betrokkenen vaak niet aan tafel zitten en de samenhang tussen incident en verbeteractie verloren gaat.
Evalueer daarom elke dag het operatiekamerproces met het gehele team de planning, misverstanden en successen. Dit kost minder dan 10 minuten per OK-programma. Organiseer voor grotere incidenten een specifieke bijeenkomst. De aansturing en cultuur zijn de verantwoordelijkheid van het volledige OKC-management. En toch, in een gezonde aanspreekcultuur geeft iedereen elkaar professionele feedback op basis van de kwalitatieve en kwantitatieve resultaten.
Plannen volgens de TIPUO-filosofie liet bij negen vakgroepen in negen ziekenhuizen een verbeterpotentieel van meer dan 15 procent van de benuttingsgraad per operatiekamer per dag zien. Dit is gemiddeld één operatie per dag of zoveel minder inzet van capaciteit. Ofwel per jaar € 1.000.000 meer inkomsten of € 300.000 minder uitgaven. Wij vinden de kortere wachtlijst voor patiënten en de prettige en efficiënte sfeer het belangrijkste resultaat. Dit resultaat borgt u door te blijven sturen, leiderschap te tonen én successen te vieren.